Table of Contents
-
What Is Migraine?
-
How Is Migraine Distinguished From Other Headaches?
-
Types of Migraine
-
Causes of Migraine
-
Symptoms of Migraine
-
How Is Migraine Diagnosed?
-
Phases of Migraine Attacks
-
Treatment of Migraine
-
Treatment to Relieve Symptoms
-
Preventive Treatment From Malaria
-
Can Migraine Be Cured?
-
Complications Involved With Migraine
-
Can Migraine Be Prevented?
-
Frequency of Migraine Attacks
-
Triggers of Migraine
-
Long Term Effects of Migraine on a Person’s Live
-
What Can You Do to Manage Migraine Better?
-
Migraine During Pregnancy, Childbirth, and Afterwards
-
Takeaway
Migraines are as unique as people themselves, with different types, triggers, symptoms, and treatments. The best way to deal with migraine is to identify and avoid personal migraine triggers. In addition, going for general-physician consultation can be helpful if frequent migraine attacks are observed.
Due to the complexity of nature and the unknown cause of migraines, learning about the migraine disorder can be intimidating. Here’s everything you need to know about this condition.
What is migraine?
Migraine is characterised as a genetically influenced neurological disorder, which causes headaches on one (or sometimes both) side of the head. The intensity of these headaches can range from moderate to severe. It is a common condition affecting roughly 1 out of every 5 women and 1 out of every 15 men; it is obvious that migraine is more prevalent in women than in men.
An episode of migraine headache is termed as a ‘migraine attack’. Generally complex in nature, migraine attacks span over a few hours to a few days, during which a person’s ability to work or perform routine tasks is reduced to a bare minimum.
Migraine, characterised by pulsating or throbbing pain in one side of the head, makes the affected person highly sensitive to external stimuli, such as light and sound. According to the Global Burden of Disease Study conducted by IHME in 2013, migraine stood out as the sixth most disabling disease.
The word ‘migraine’ originated from ‘hemikrania’, which is a term used in ancient Greek (where ‘hemi’ means half, and ‘kranion’ stands for skull). It was later converted into Latin as ‘hemigranea’, which translates to ‘migraine’ in French.
How Is Migraine Distinguished From Other Headaches?
The main difference between migraine and other headaches is the type of pain. Migraine headaches are characterised by a pulsating pain that usually covers one half of the head, whereas regular headaches can be felt evenly on both the sides of the head.
Another key difference is the symptom; some people experience an aura before the pain actually begins. Migraine headaches can also be episodic in nature, which means that they occur frequently (perhaps once every week) or may be triggered by external stimulation.
Migraine headaches require medical diagnosis by a doctor who may request an MRI or a CT scan to confirm the condition.
Types of migraine
As mentioned earlier, migraine is a complex condition that is divided into different categories.
Please note that everyone may not have a typical type of migraine. If you have any doubts about your condition, it is best to consult a doctor.
Migraine with aura
In this type of migraine, people have a warning (often referred to as an ‘aura’) before the actual headache starts. One in every three individual experiences an aura before the migraine attack. A person with this type of migraine would commonly see flashing lights, coloured spots/patterns, or have momentary blindness during an aura.
The following are the subtypes of migraine with aura:
Migraine with brainstem aura
This type of migraine develops gradually over time in people. Formerly known as basilar-type migraine, it is often accompanied by the following symptoms:
1. Vertigo
2. Slurred speech
3. Ringing in the ears
4. Double or blurry vision
5. Dizziness
6. Confusion
7. Disorientation
Few people may also experience temporary loss of consciousness (or syncope). Symptoms associated with migraine with brainstem aura may first occur in adulthood.
Hemiplegic migraine
This is a rare condition in which one side of the body goes under temporary paralysis. Hemiplegic migraine may or may not be followed by headache. The symptoms of hemiplegic migraine include:
1. Tingling sensation and temporary weakness in one side of the body
2. Dizziness or confusion
3. Ringing in the ears or hearing problems
4. Visual disturbances (seeing coloured spots or sparkles)
5. Speech difficulties (unable to speak properly)
6. Difficulty in written and verbal communication (problems encountered with listening, speaking, reading, and writing)
The weakness generally subsides within 24 hours. People may or may not get headache in this type of migraine, but the overall experience can be frightening.
Retinal migraine
In this type of migraine, the person may experience temporary blindness (that lasts for 10–20 minutes) in one eye besides headache. The eyesight of a person goes back to normal after the migraine attack. Some people get retinal migraine attacks every month; however, the frequency may vary.
Partial or total loss of vision in one eye is a distinguishing factor of retinal migraine (also known as ocular migraine). Most people report that the same eye is affected during every visual attack.
Migraine without aura
As the name suggests, migraine without aura (formerly known as common migraine) comes without a warning sign. This is a common type of migraine that affects individuals for 4–72 hours, generally on one side of the head. Migraine without aura can be aggravated by a physical activity and can be accompanied by nausea. The frequency of these attacks may vary from once every few years to several times a week.
Status migrainosus
It is associated with extreme pain and nausea that can last for more than 72 hours, and this condition doesn’t respond to migraine treatment easily. Status migrainosus is a severe type of migraine that may also require a hospital visit. Stress, certain medication, changes in your medication, or even weather changes can trigger status migrainosus.
Migraine without head pain
Previously known as ‘acephalgic migraine’, migraine without head pain starts with an aura phase but does not involve any headache. Hence, it is also commonly known as ‘silent migraine’.
Causes of migraine
Science suggests that multiple impairments of primary neurones lead to a series of subtle changes in and outside the brain that cause migraines. These changes may occur in the brainstem (base of the brain) and during its interactions with the trigeminal nerve (a major pain pathway). Serotonin, released from the brainstem region, may also play a role in migraine.
The elevated level of some neuropeptides, including calcitonin gene-related peptide (CGRP), have been found in the spinal fluid of chronic migraine patients. This information implies that genetic composition is a huge factor in migraine.
However, causes of this complex condition are not clear yet; research is still being conducted to get to the root cause of migraine.
Symptoms of Migraine
Throbbing or pulsating pain with a moderate to severe intensity is the primary symptom of migraine. They are usually one-sided but may also affect any part of the head, face, and neck. Few people complain about increased sensitivity to noise, light, and/or odour in their surrounding during a migraine attack.
Some physical activities are known to make migraine worse by intensifying nausea and other symptoms and by disrupting a person’s daily routine. In some cases, migraine pain can transcend to the face or neck—where it can be confused with arthritis or a sinus headache.
Migraine symptoms other than headache include the following:
1. Vertigo
2. Loss of appetite
3. Fatigue and dizziness
4. Nausea and/or vomiting
5. Blurred vision
6. Tender scalp
7. Excess sweating or chills
8. Pale skin colour
Few rare symptoms of migraine include:
1. Diarrhoea
2. Fever
3. Temporary partial/complete blindness in one eye in some cases
4. Temporary paralysis on one side of the body
5. Reduced cognitive capacity especially for communication
How Is Migraine Diagnosed?
The less severe cases of migraine are often undiagnosed because people may pass them off as regular headaches due to over-exertion or a common cold. In addition, few people experience symptoms similar to a sinus headache, including nasal congestion, watering eyes and even facial pressure, making it even highly complicated to diagnose migraine.
It is recommended to keep a track of regular or episodic migraine headaches, accompanying symptoms, and administered migraine treatment. Take this information and consult a doctor to discuss the possibilities. Regular headaches, even if they are mild in intensity, should not be taken lightly.
It is best to consult a doctor, in case you notice a change in the pattern or the condition, even if you have been diagnosed with migraine before or have a history of migraine headaches. If the doctor suspect migraine, they will fish through a person’s and their family’s medical histories. Additionally, the doctor will likely ask the patient to go for imaging tests (such as MRI or CT scan) and blood tests to rule out other possibilities. The doctor may also request an electroencephalogram (EEG) if there are symptoms similar to a seizure.
The following information can help with the accurate diagnosis of migraine:
1. Frequency of headaches
2. Time duration of headache and other symptoms
3. Potential triggers
4. Type and location of pain
5. Effects of external stimulation on headache—both good and bad
6. Lifestyle
7. Medication taken to calm the pain
8. Whether any family member has migraine
A person should seek immediate medical attention if any of the following sings and symptoms are observed:
1. Abrupt severe headache
2. Troubles with vision
3. Weakness or numbness in any part of the body
4. Stiff neck and/or confusion
5. Fever
6. Recent head injury that led to a headache
7. Severe headache that increases in intensity with physical activity
8. New headache after the age of 50
Phases of migraine attacks
A migraines attack is divided in four stages based on the symptoms and other aspects of a person’s health. It can take a person approximately 72 hours to go through all four stages.
Prodrome—first stage
Also known as the ‘pre-monitory’ or ‘pre-headache’ phase, the first stage usually stretches over a few hours or sometime a few days. Generally, a person starts experiencing the following symptoms one or two days before a migraine attack:
1. Increased urination
2. Constipation
3. Sudden mood swings
4. Food cravings
5. Neck stiffness
6. Water retention
7. Frequent yawning
Aura—second stage
This is more of a warning stage that usually starts before the headache (but sometimes strikes during the headache). An aura mostly consists of visual disturbances and other reversible symptoms of the nervous system that build up gradually and lasts for up to 60 minutes.
Common symptoms of an aura include the following:
1. Blind spots
2. Seeing flashes of lights
3. Seeing coloured spots or patterns
4. Temporary blindness
5. Tingling sensation or numbness in parts of the body
6. Dizziness and weakness
Migraine headache is preceded by an aura in up to 25% patients. Some people experience auras without headaches.
Headache—third stage
This is the most prominent stage for most people as the throbbing pain can be excruciating sometimes. The headache can last anywhere from 4–72 hours. It is very likely that the person who in this stage will not be able to perform most of their routine tasks. People also complain about nausea and sensitivity to sound, light, and/or odour in this stage.
Postdrome—fourth stage
Often referred to as a ‘migraine hangover’, this stage is experienced by most people who have migraine. It can go on for a day or two after the headache stops, and sudden head movements might bring brief pain. People report feeling dull, elated, or confused with inability to concentrate.
Treatment of migraine
The severity of symptoms along with the frequency and duration of migraine attacks determine the treatment for an individual. The right treatment prevents future attacks and stops symptoms, whereas improper migraine treatment can cause intermittent migraines to become chronic migraines.
Drugs mentioned below are designed for treating migraine. However, one should always opt for general physician consultation before taking any of these drugs.
Treatment to relieve symptoms
Pain-relieving medication is taken to stop (or at least minimise) a migraine attack. This type of migraine treatment is also known as abortive or acute treatment. A person with migraine should take these medicines as soon as they observe first signs of migraine for maximum efficiency. General medicinal recommendations by doctors include the following:
Pain relievers: They include prescription pain relievers or over-the-counter drugs, such as aspirin or ibuprofen. It is important to note that these may lead to medication-overuse headaches, ulcers, or gastrointestinal bleeding, when taken for too long.
Triptans: Rizatriptan and sumatriptan are some of the prescription drugs that block pain receptors and are used to treat migraine. Doctors might prescribe other drugs to people at the risk of a heart attack or stroke.
Dihydroergotamine: This drug works best for migraine attacks that last for more than 24 hours, when taken soon after the symptoms start showing. Dihydroergotamine is available in the form of a nasal spray or injection. It is not suitable for people with high blood pressure, coronary artery disease, kidney ailments, or liver diseases.
Lasmiditan: A new tablet, lasmiditan can considerably improve migraine headaches. People should rest at home after taking this medication as it can have a sedative effect.
CGRP antagonists: This prescription drug can alleviate pain and nausea and reduce sensitivity to light and sound in about 2 hours. Oral CGRP antagonists such as rimegepant and ubrogepant have been recently approved for treating adults who have migraine with or without aura. Dry mouth and excessive lethargy are common side effects of this drug. These drugs shouldn’t be taken with strong CYP3A4 inhibitor drugs.
Opioid medications: These drugs are sought as the last resort for people who are not benefitting from any other form of treatment, as they can be highly addictive.
Anti-nausea drugs: People who experience severe symptoms of nausea and vomiting are advised to pair drugs, including metoclopramide and chlorpromazine, with pain relievers.
Preventive Treatment From Malaria
Preventive treatment is the best strategy to treat severe migraine that is frequent, long lasting, and/or accompanied by neurological symptoms. Along with daily prescription medicines, the doctor might urge dietary modification with vitamin supplements and changes in lifestyle.
This approach aims to reduce the frequency, duration, and severity of the migraine attack. The following options are often prescribed:
Drugs for lowering blood pressure: These include beta blockers such as metoprolol tartrate and propranolol. For people who have migraine with aura, calcium channel blockers such as verapamil may be prescribed.
Antidepressants: Amitriptyline is a tricyclic antidepressant that helps in preventing migraine attacks. However, other antidepressants might be prescribed instead of amitriptyline because it makes people lethargic.
CGRP monoclonal antibodies: Drugs including eptinezumab-jjmr (Vyepti), galcanezumab-gnlm (Emgality), and fremanezumab-vfrm (Ajovy) can be given intravenously on a monthly or quarterly interval. These are all relatively new drugs for treating migraine that have been approved by the Food and Drug Administration. A common side effect reported by individuals on these drugs is a reaction at the injection site.
Anti-seizure drugs: Topiramate and valproate might be helpful to people with less frequent migraine attacks. Some common side-effects of this drug include nausea, dizziness, and weight changes. These drugs are not suitable for pregnant women or women who are trying to conceive.
Botox injections: Some adults, who have been administered injections of onabotulinumtoxinA (botox) approximately every 12 weeks on a doctor’s recommendation, have found the treatment beneficial.
Please note: Drugs listed here are only for providing information. You must always seek a doctor’s approval before taking any medication to avoid mishaps.
Can migraine be cured?
As of now, there is no cure for a complex condition such as migraine. It is safe to assume that a viable cure for migraine will be available only after the root cause of migraine is discovered.
Biofeedback is a revolutionary method of therapy that helps people control some of their bodily functions at will. This mind-body therapy can greatly impact a person’s mental and physical health.
Complications involved with migraine
Migraine, already a complex disorder, when coupled with another ailment can be challenging to bring under control and treat. The following are some of the known migraine complications:
1. Status migrainosus: It is a severe intensity migraine that lasts more than 72 hours and debilitates the affected person.
2. Persistent aura without infarction: This condition can go undetected on neuroimaging for 1 week or beyond. The individual experiences aura symptoms throughout in this.
3. Migrainous infarction: It includes one or more aura symptoms related to brain ischemia on neuroimaging during a typical attack.
4. Migraine aura-triggered seizures: As the name suggests, in this condition the aura of a migraine attack triggers a seizure.
Apart from these, migraine is also associated with a very small risk of mental health problems, such as panic disorder, anxiety disorder, bipolar disorder, and/or depression.
Studies have also shown that people with migraine (especially those who experience aura) are roughly at twice the risk of having an ischaemic stroke in comparison with people without migraine. In addition, using combined contraceptive pills also increases the risk of women, who have migraine with aura, of having this stroke.
Can migraine be prevented?
Although a person cannot avoid having migraine, they can surely prevent migraine attacks or delay them at the very least. As discussed before, people who have frequent migraine attacks of severe intensity are given preventive migraine treatment. Besides, one can identify triggers and avoid them to prevent a migraine attack.
Who is prone to having migraine?
Since migraine is known to be a genetic disorder, people who have family history of migraine are prone to having the disease. Several factors affect your chances of having migraine; these factors include:
1. Age: Generally, the first occurrence of migraine is in the adolescent years of a person, and migraine tends to hit peak during 30s. After this, the intensity and frequency of migraine attacks gradually decrease.
2. Gender: Women are thrice as likely as men to get migraine.
3. Hormones: Migraines are especially troublesome for women. They may notice changes in migraine attacks before or after menstruation, during pregnancy, or around menopause. Migraine attacks usually become less bothersome after menopause.
Frequency of migraine attacks
Depending on a person, migraine attacks can be as frequent as few times a week or as rare as once or twice a year. Preventive medication, alternative therapy, and/or lifestyle changes might be recommended by a doctor after a general-physician consultation to reduce the frequency of migraine attacks.
Triggers of migraine
The cause of migraine is uncertain, but through research, several triggers have been identified. Some common triggers of migraine are listed below; however, theses can vary from individual to individual.
1. Many women have reported a pattern of migraine headaches around menstruation cycles, pregnancy, and menopause. These are linked to fluctuations in oestrogen levels in the body.
2. Medications that interfere with the body’s hormonal balance, such as contraceptive pills, can intensify migraine attacks.
3. Caffeine and alcohol, especially wine, are both identified as triggers for migraine.
4. Stress in work or personal life can also induce migraines.
5. Changes in the sleep cycle, sleeping too much or too little, can trigger migraines in few individuals.
6. Intense physical activity, including a strenuous workout routine or increased sexual activity, triggers migraine in some people.
7. Sudden changes in the weather or atmospheric pressure can also induce migraine.
8. Loud sounds, strong smells, or bright/flashing lights can invoke migraine attacks in some people. People become especially sensitive to sensory stimuli during the aura phase.
9. Too much consumption of pain relievers has been linked to medicine-induced migraines.
10. Skipping meals or fasting may trigger migraine in some individuals, so might consuming processed foods and aged cheese.
11. Food additives such as monosodium glutamate or MSG (a preservative) and aspartame (a sweetener) can trigger migraines.
It is unclear as to why sometimes any of the aforementioned triggers may induce migraine and sometimes none of them may show any effect. Besides, an individual may have different triggers than what are mentioned here, which is why it is important to track migraine attacks and related symptoms all the time. Tracking through a migraine journal can help a person better manage their migraine.
Long term effects of migraine on a person’s live
If left untreated for long, moderate migraines can develop into more severe and chronic migraine. In addition, studies have found that having migraine for a large portion of one’s life can lead to other co-morbidities.
During early diagnosis, migraines are often linked to depression, anxiety, and panic disorders. Some people also develop sensory problems like photophobia. There’s also a high risk of migraine leading to stroke in people who are 50 or older.
Migraine can be a serious condition that restricts a person from going about their lives and may disrupt a person’s routine and work for days. In worse case scenarios, people experience extreme symptoms and are forced to stay at home and rest. Not to mention, this disease affects a chronic migraine patient’s social life significantly.
What can you do to manage migraine better?
Even if there is no cure to migraine yet, there are numerous things you can do manage the condition better.
1. Tracking—migraine journal
Migraine symptoms and triggers are different for everyone and, usually, so is the treatment. Keeping a track of migraine in a designated journal can be extremely beneficial; one can learn about their triggers, and their doctor can learn about what works and what doesn’t to treat the condition. Include everything in detail about all migraine attacks:
a. When did it start/end? (Add information about different phases if possible)
b. What are the symptoms?
c. Sleep schedule around migraine attack.
d. Potential triggers—any changes in schedule or diet, special events attended, etc.
e. Is there a pattern?
f. Is the patient under stress? What is the reason for stress?
g. How is the weather?
h. Intensity of the pain on a hedonic scale (1 to 10).
i. Location of the pain
j. What medicines were taken before attack?
This journal does not have to be a physical one; one can use notes in their phone for tracking.
2. Alternative therapies
Acupuncture, biofeedback, and cognitive behavioural therapy can be helpful in relieving chronic pain.
3. Home remedies
Practising meditation and yoga on a regular basis can relieve stress (a common migraine trigger); this in turn helps in reducing the duration and frequency of migraine attacks. In addition, the following are helpful in reducing symptoms during a migraine attack:
a. Rest in a quiet and dark room
b. Nap
c. Drink plenty of water
d. Apply a cold compress to forehead or back of the neck
e. Scalp massages or applying pressure to the temples
f. Deep breathing to remain calm
4. Lifestyle
Since many migraine triggers are lifestyle changes, maintaining a proper routine can be helpful. Set and follow a manageable routine that promotes healthy habits such as sleeping, waking, and eating meals at the same time every day. Regular exercise reduces stress and may be helpful; however, be mindful not to overexert.
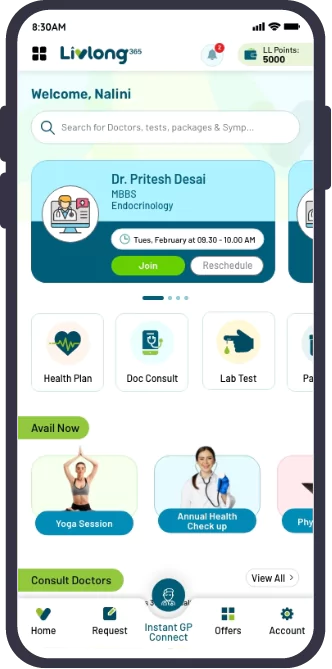
5. General-physician consultation
Migraine is indeed a complex condition with unknown causes and no prominent cure. It is recommended that people with migraine (especially who experience aura symptoms) should go for basic full body check-up once in a while after general-physician consultation to ensure optimum health and detect any complication early on.
Migraine during pregnancy, childbirth, and afterwards
As noted earlier, migraine can be triggered by hormonal changes; not all medicines can be used during the time of pregnancy or while breastfeeding. It is important for expectant or new mothers to be cautious of the migraine treatment they take.
1. Alternative therapies should be used to prevent migraine attacks
2. Minimum use of medicines is recommended
3. Identify and avoid potential migraine triggers
4. A doctor may recommend a less potent painkiller (for example paracetamol) when necessary
5. Anti-inflammatory medicine or triptans may be advised for some people
General-physician consultation before taking any medicine for migraine is advisable during pregnancy or breastfeeding stages.
Takeaway
Migraine can have a huge impact on a person’s quality of life and turn daily routines such as bathing and cooking a tiresome feat. Though the actual cause of this genetic neurological disorder is not evident yet, ongoing research may shed some light on how to cure migraine in the future.
Even though effective treatments to prevent and relive symptoms are available, it is best to go for a general-physician consultation before self-medicating as diagnosing migraines is very tricky. It is likely that migraine attacks will worsen over time if left untreated. Identifying potential migraine triggers, keeping track, and avoiding them is the best way to prevent future attacks. Migraine also tends to gradually decrease in intensity and frequency over the years for most people.